Adeptia helps clients increase their clear rate by identifying and correcting Claims errors before they are processed. In addition, our ability to support human workflow allows your business users to quickly identify, correct, and resubmit Claims in minutes. Together Adeptia’s Claims data onboarding solution allows our clients to unlock millions of dollars in Claims that traditional solutions lose sight off.
Our insurance integration solutions is meant for your business users to configure client onboarding, map data, fix data errors through workflows and track inbound and outbound transmissions of Claims.
Companies that provide Billing solutions to Payers and Healthcare Providers often do much of the data onboarding manually or hand it off to IT. Problem with this type of insurance integration is that it limits the amount of service that vendors can offer to their customers and the slow process creates a huge backlog of Claims that are untouched for months or years. A vendor gets paid from the client when the HIPAA 837 Claims information is successfully sent to the Payer.
Errors in processing delays vendor’s revenue. In order to be able to scale up the business, to process the claims data more effectively and to generate quicker revenue, Adeptia has developed an insurance integration software that enables Healthcare vendors the automation required to receive Claims from the clients, apply business rules and send valid Claims to the Payers.
Adeptia’s Claims data onboarding automates and accelerates your billing processes which are often obstructed by data integration challenges that require IT rather than Business to fix these Claims such as getting the data from backend systems, understanding the errors and applying business rules to fix them before sending them to Payers. And all these tasks require weeks of back-and-forth between IT and Business to discuss and formulate a plan of action to resolve these issues which further delays revenue.
The key reason for this disconnect is that organizations often choose a technical tool to fix what is essentially a business problem. IT custom codes or uses a very technical “engineering-centric” toolset (that only they know how to use) in order to fix the data errors and the code needs to be constantly updated and retested whenever a new set of data errors or a specific Payer related issues are encountered.
Backlogged HIPAA 837 Claim applications that require corrections related to incorrect Social Security Numbers, incorrect Provider IDs require different validation rules that business typically requests IT to perform which takes weeks or months to fix. Validation rules can be per client or type of message. The tasks related to managing Claims processing becomes an IT function rather than a business function. Additionally, the schemas of the HIPAA 837 Claim may need to be tweaked for a particular Payer to handle their custom field or a segment.
Because of acquiring these technical toolsets, such as eclipse based desktop tools, business cannot perform these functions on their own and waits for IT to respond to their requests that can take months to resolve. Business cannot bill their clients until they are able to fix and send Claims to Payers. The entire revenue model is based on IT’s resource availability and priorities.
Ask this simple question, who are the custodians of the Claims onboarding and billing process? Is it business or IT or both? We think it’s both. We at Adeptia believe that business should be able to perform business functions through a simple, graphical user interface that allows them to access incoming or backlogged Claims, apply validation rules and utilize human workflows to review and correct data or reconciliation errors before sending them to Payers.
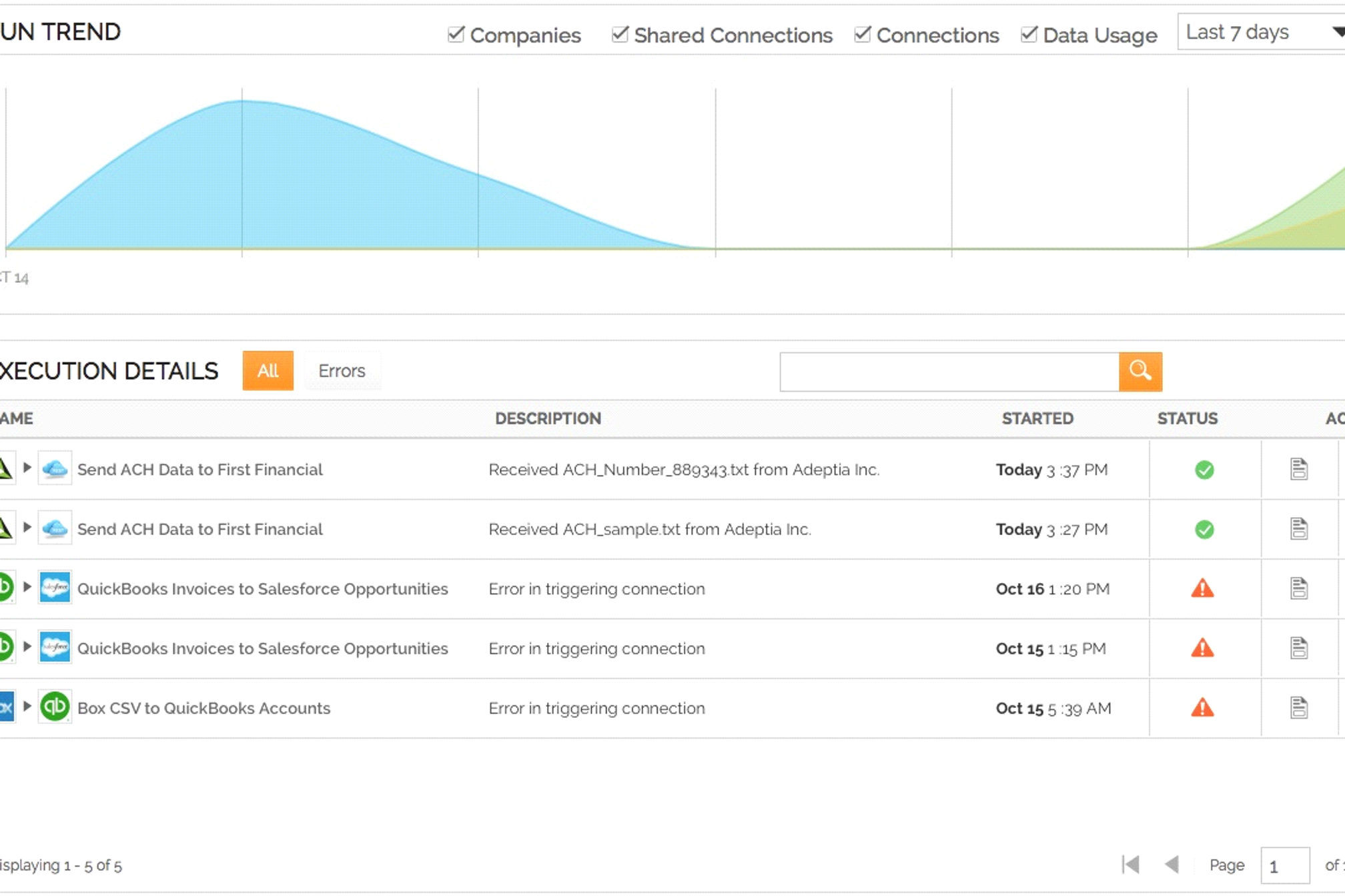
Additional features such as dashboards to track pending Claims that are flagged as exceptions with detailed error descriptions also play an important role in helping business deliver their services quickly and expedite the billing process. IT plays an important role in data governance by securing and providing access to the data.
Adeptia’s Claims Data Onboarding Solution consists of the following features.
1. Adeptia Connect – B2B Portal to onboard Claims data
The first thing we solve is making it easy for your business to onboard Claims data from your new or existing clients. Adeptia Connect is a secure cloud-based B2B Portal that lets companies publish and share data connections with your business network. Your clients simply discover and consume these connections from the cloud marketplace in minutes. In other words, your company establishes a HIPAA 834 Claims data connection and your client is able to see that connection and subscribes to it through a self-service wizard and is able to send the data you need in minutes.
Learn more about Adeptia Connect features & benefits. Also, refer to videos on how to use Adeptia Connect.
2. Adeptia Integration Suite – B2B integration platform for business users
Adeptia Integration Suite is not a developer tool, but a true business solution. Our goal is to upend the traditional paradigm of integration software, namely, that it is a developer tool for IT teams to use. We want AIS to be recognized as a business application for exchanging business data, a key part of running a business.
Using AIS, users can connect to backend databases, pull out Claims data and can apply business rules and generate a valid HIPAA 837 Claims file. Now you no longer need to wait apply those cross-reference service codes, fixing the SSN that has dashes, or the missing Provider ID or any other data issues that you want to fix.
Drag and drop graphical mapper allows you to pull data and apply Claims 837 mapping rules.
Here are some videos on how to apply data mapping rules in Adeptia Integration Suite’s Mapper interface.
Automate the entire end-to-end process of onboarding, processing and managing Claims to Payers through a Trading Partner interface.
Build pre or post process workflows to cleanse data or route the Claims to other backend systems. AIS provides full workflow orchestration capability through its Process Designer interface.
Here is a video on how to design a process flow.
3. Accelerated Claims Capture – a business application for Operations to manage Claims data
Adeptia provides rich and holistic management front-end templates for tracking and managing Claims. With the help of Adeptia’s consultation services, this interface can be customized to your preference. It has the ability to report on the data in a grid, user can select a Claim and make modifications. This application runs on top of the AIS and gives an added abstraction layer to your business team who can focus on the data and not on the underlying mappings and processes that are supporting the Claims Billing Solution.